Table of Contents
ToggleNon-IGE-Mediated Food Allergies: Culinary Delights to Dangers
Imagine indulging in the delectable wonders of the culinary world, savoring each bite, only to find that your body rebels against the very sustenance that brings joy to millions.
Such is the unfortunate reality for individuals grappling with food allergies.
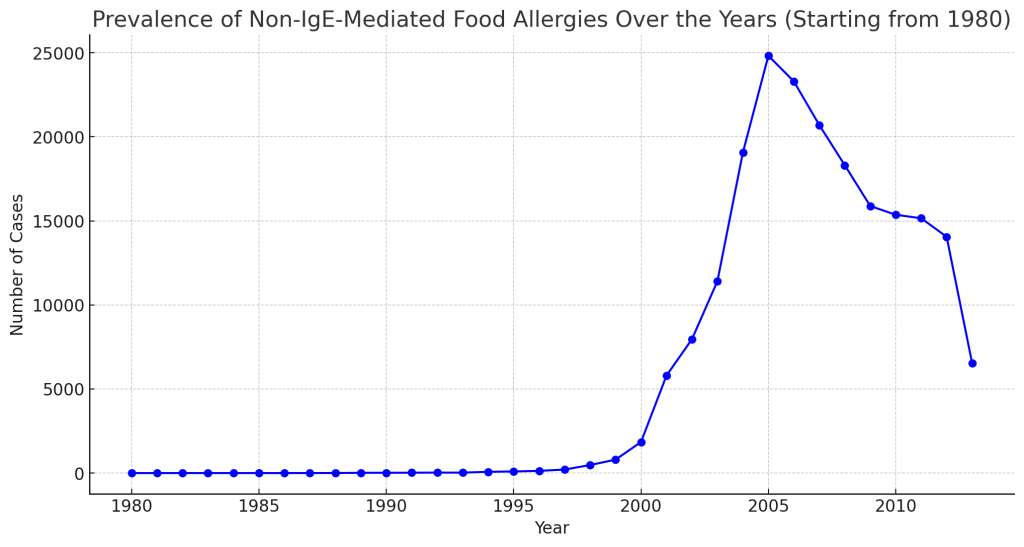
In recent years, these immune-mediated reactions have garnered significant attention due to their wide-ranging effects on health and quality of life.
The Mystery of Non-IGE-Mediated Food Allergies
You probably know about common food allergies that cause immediate reactions like hives or anaphylaxis. These reactions happen because of something called IgE.
Another type of food allergy, called non-IgE-mediated food allergies, is gaining recognition.
These allergies don’t show their symptoms right away, confusing both patients and doctors alike.
Different kinds, such as Food Protein-Induced Enterocolitis Syndrome (FPIES) and Food Protein-Induced Allergic Proctocolitis (FPIAP), fall under these non-IgE food allergies.
Unlike immediate allergies, FPIES and FPIAP take time to show symptoms, mainly affecting the digestive system.
It’s essential to learn about and understand these allergies to diagnose and manage them correctly, and to get a clearer picture of our diverse immune system.
Understanding FPIES (Food Protein-Induced Enterocolitis Syndrome)
Definition and Symptoms of FPIES:
FPIES, or Food Protein-Induced Enterocolitis Syndrome, is a non-IgE-mediated food allergy that primarily affects infants and young children.
It is characterized by delayed allergic reactions to certain foods, typically occurring within hours after ingestion.
Unlike IgE-mediated allergies that primarily involve the immune system’s immediate response, FPIES triggers a delayed immune response in the gastrointestinal tract.
Symptoms of FPIES include severe vomiting, repetitive retching, diarrhea (sometimes with blood), dehydration, lethargy, and in some cases even shock.
These symptoms can be extremely alarming for parents who may initially suspect a stomach virus or food poisoning.

Mechanism of FPIES Reaction in the Gut
The exact mechanism behind FPIES is not fully understood yet, but researchers believe it involves an abnormal immune response within the gut mucosa.
When a trigger food is ingested by an individual with FPIES, it leads to an inflammatory reaction in the small intestine.
This inflammation causes increased permeability of the intestinal lining and triggers the release of various pro-inflammatory molecules.
As a result, fluid builds up in the intestines leading to vomiting and diarrhea. The intestinal cells also become inflamed which impairs their ability to absorb nutrients properly.
Common Foods That Trigger FPIES
Foods that most commonly trigger FPIES reactions vary depending on geographical regions and individual sensitivities.
However, there are some common culprits that have been identified worldwide.
- Cow’s milk protein
- Soy protein
- Grains (e.g., rice, oats)
- Poultry
- Eggs
- Fish
Note: Trigger foods can vary for each individual, and some may have multiple triggers. The protein components in these foods often cause the reaction.
Diagnosis & Management of FPIES
Figuring out if someone has FPIES is tough because its signs take time to show up and can be vague.
Usually, doctors look at a person’s medical history, symptoms, and how they react to certain foods and diets to make a clear diagnosis.
If someone does have FPIES, staying away from foods that cause reactions is crucial to avoid more problems.
This might mean moms who are breastfeeding may have to change their diets, or babies on formula might need special hypoallergenic ones.
It’s also important to teach parents how to handle serious reactions and make sure they get medical help fast when needed.
Exploring FPIAP (Food Protein-Induced Allergic Proctocolitis)
Definition and Symptoms of FPIAP
Food Protein-Induced Allergic Proctocolitis, or FPIAP for short, is a mouthful to say but a condition that affects the lower gastrointestinal tract of infants.
Unlike other non-IgE-mediated food allergies, such as FPIES, which affect the entire gastrointestinal tract, FPIAP focuses its wrath primarily on the colon and rectum.
Symptoms can vary from mild to moderate, with affected infants experiencing frequent episodes of bloody stools, often accompanied by mucous or even occasional diarrhea.
The stool may appear greenish or brownish in color due to the presence of blood in the digestive system.
While it may sound alarming to new parents, rest assured that FPIAP is generally not associated with severe complications or life-threatening reactions.

FPIAP vs Other Non-IgE Food Allergies Differences
What sets FPIAP apart from its counterparts like FPIES is its limited focus on the lower part of the digestive system.
While both conditions share some common symptoms such as diarrhea and vomiting, it’s crucial to distinguish between them due to their different target areas within the gut.
Unlike other non-IgE-mediated food allergies which can present with delayed symptoms hours after ingesting trigger foods, symptoms of FPAIP typically appear within 1-2 hours after consumption.
Trigger Foods in Breastfed vs Formula-Fed Infants
Foods that provoke allergic reactions in infants with FPAIP can vary depending on whether they are breastfed or formula-fed.
In the case of breastfed infants, the mother’s diet plays a significant role. Common culprit foods include cow’s milk protein, soy, and eggs.
It is important for nursing mothers to be cautious and observe any changes in their baby’s stool patterns or overall well-being after consuming certain foods.
On the other hand, for formula-fed infants, the trigger foods are often found in specific formulas themselves.
Some of these may contain proteins derived from cow’s milk or soy. If your little one is diagnosed with FPAIP, your pediatrician may recommend switching to hypoallergenic formulas that are specifically designed to minimize allergic reactions.

Diagnosis and Management of FPAIP
Figuring out FPAIP in a baby is tough because its symptoms often mimic other stomach problems.
A knowledgeable doctor will ask detailed health questions and conduct tests to confirm the condition. If a baby has FPAIP, changing their diet usually helps.
Breastfeeding moms may need to modify their diets to avoid problem-causing foods, ensuring they and their babies still get proper nutrition.
For formula-fed babies, a switch to a special kind without certain proteins might work.
If diet changes don’t help, or symptoms are severe, the doctor will recommend other treatments or refer the baby to a special allergy clinic. Understanding FPAIP and its management helps keep babies healthy and happy.
Shared Symptoms and Clinical Presentations Between Conditions
When it comes to non-IGE-mediated food allergies like FPIES (Food Protein-Induced Enterocolitis Syndrome) and FPIAP (Food Protein-Induced Allergic Proctocolitis), there are some shared symptoms that can make diagnosis a tricky task.
Both conditions exhibit gastrointestinal symptoms such as vomiting, diarrhea, and abdominal discomfort.
Affected infants may display poor weight gain, irritability, and in severe cases, even failure to thrive. These shared clinical presentations often leave medical professionals scratching their heads initially.

Factors: Age of Onset, Severity, and Resolution Patterns
So, FPIES and FPIAP got some things in common but there are ways to tell them apart. Like, FPIES usually starts when a baby begins to eat solid food.
But FPIAP shows up in the first few months after a baby is born when they’re exposed to food allergens from breastfeeding or formula.
Both can be from not so bad to really bad, but FPIES is known for causing serious vomiting that can lead to dehydration or even shock-like symptoms.
On the other hand, FPIAP mostly causes blood in the stool or diarrhea filled with mucus, without causing other big health problems.
How these conditions go away is different. Most kids outgrow both by the time they’re three or four years old, but it seems like kids with FPIES usually get over their allergy quicker than those with FPIAP.
Mechanisms Behind Non-IGE-Mediated Food Allergies
Role of T-Cells in Non-IGE-Mediated Reactions
The immune system plays a central role in non-IGE-mediated food allergies like FPIES and FPIAP, with T-cells taking center stage.
In these conditions, specific food proteins activate T-cells, triggering an immune response that leads to inflammation in the gastrointestinal tract.
Unlike classic IgE-mediated allergies, this response does not involve the production of specific antibodies (IgE), making it challenging to diagnose using traditional allergy tests.
The Role of Cytokines in Gut Inflammation
Cytokines from immune cells notably enhance the inflammatory cascade in non-IGE-mediated food allergies.
Cytokines such as IL-4, IL-5, and TNF-alpha play a crucial role in amplifying the immune response and promoting inflammation within the gut.
Genetic Predisposition to Certain Food Allergies
It is widely believed that genetic factors play a role in determining an individual’s susceptibility to develop non-IGE-mediated food allergies.
Certain genetic variations have been identified that may increase an individual’s likelihood of developing FPIES or FPIAP. However, more research is needed to fully understand the complex interplay between genetics and environmental triggers.

Long-Term Outlook for Non-IGE-Mediated Food Allergy Patients
Impact on Growth, Development, and Nutrition
Non-IGE-mediated food allergies can have long-term implications for affected individuals.
Prolonged restrictions on certain foods can potentially impact their growth and development if appropriate nutritional substitutes are not provided.
Close monitoring by healthcare professionals is crucial during this period to ensure optimal nutrition and support healthy growth.
Managing Dietary Restrictions with Adequate Nutrition
Managing dietary restrictions in individuals with non-IGE-mediated food allergies requires a comprehensive and individualized approach.
Healthcare professionals, dietitians, and families must collaborate to create balanced meal plans, addressing nutritional gaps and avoiding trigger foods.
Innovative solutions such as hypoallergenic formulas or alternative protein sources may be considered when necessary.
Current Research Efforts on Understanding
The scientific community continues to make strides in comprehending the intricacies of non-IGE-mediated food allergies.
Ongoing research efforts aim to improve diagnostic methods, uncover novel treatment options, and gain a deeper understanding of the underlying mechanisms driving these conditions.
The hope is that with further advancements in knowledge, effective interventions can be developed to alleviate the burden faced by those affected by FPIES and FPIAP.
A Word from HealthyVibe
Non-IGE-mediated food allergies like FPIES and FPIAP are tough to figure out, but they also give doctors and researchers a big chance to learn.
These allergies can look the same at first, but doctors can use when they start, how bad they are, and how long they last to tell them apart.
A lot of ongoing research aims to increase our knowledge in this area. This research offers hope for better diagnosis and treatment of these allergies, improving life for those living with non-IGE-mediated food allergies.











