Table of Contents
ToggleFood Allergies vs. Food Sensitivities
Food allergies and food sensitivities are often used interchangeably, but it is important to understand the distinctions between these two terms.
A food allergy is an immune system response triggered by the consumption of a specific food.
People with a true food allergy have immune systems that recognize certain food proteins as threats.
Their bodies produce an antibody, immunoglobulin E (IgE), to combat these proteins.
This IgE-mediated response leads to the release of histamine and other chemicals in the body, causing allergic symptoms.
Food sensitivities refer to adverse reactions to certain foods that do not involve the immune system.
These reactions can be caused by various mechanisms such as enzyme deficiencies or chemical intolerances. Unlike food allergies, food sensitivities may have delayed onset, making it more challenging to identify the trigger food.
Allergies tend to be more severe and potentially life-threatening compared to sensitivities.
Food allergies can manifest in various ways including hives, itching, swelling of lips or throat, vomiting, diarrhea, difficulty breathing, or even anaphylaxis—a severe allergic reaction that requires immediate medical attention.
Symptoms of food sensitivity include digestive issues like bloating or diarrhea as well as headaches or skin problems like eczema.

Prevalence
The prevalence of food allergies and eczema has been steadily increasing in recent years, causing concern among healthcare professionals and researchers.
Studies suggest that food allergies affect approximately 6-8% of children and 2-4% of adults globally. These numbers can vary considerably depending on geographic location, age group, and other factors.
In the case of eczema or atopic dermatitis, its prevalence is even more widespread.
It is estimated that around 15-20% percent of children worldwide experience symptoms of this chronic inflammatory skin condition at some point during their childhood years.
Eczema can persist into adulthood in approximately 2-3% percent of individuals as well.
Symptoms
Food allergies and eczema can often present with a range of symptoms, both individually and in combination.
Food Allergy Symptoms:
- Itching:
- May occur both inside (in the mouth or throat) and on the skin.
- Skin Reactions:
- Individuals may develop hives or a rash.
- Rashes may be red, raised, and intensely itchy.
- Swelling:
- Individuals may experience swelling of the lips, face, tongue, or throat.
- Seek immediate medical attention for this symptom.
- Gastrointestinal Distress:
- Individuals may experience abdominal pain, cramping, nausea, vomiting, or diarrhea.
- Anaphylaxis:
- Individuals may have difficulty breathing due to airway constriction and a drop in blood pressure.
- Treat this as a medical emergency and administer epinephrine via an auto-injector immediately.
Eczema Symptoms:
- Itching:
- Remains a predominant symptom with or without food allergy triggers.
- Affected Skin Appearance:
- Skin may appear dry, scaly, red, and inflamed.
- The skin may have raised bumps (papules), ooze fluid (exudate), and crust over time when scratched excessively.
- Properly manage skin to prevent secondary infections.
Causes
While the exact causes may differ from person to person, research has shed light on several potential factors that contribute to the development or exacerbation of food allergies and eczema.
Genetics plays a significant role in both food allergies and eczema.
Research has identified certain genetic variations that may increase the risk of developing allergic diseases, including food allergies and eczema.
These genetic factors affect how our immune system responds to specific allergens, making some individuals more susceptible to allergic reactions.
Another important factor contributing to food allergies and eczema is an abnormal immune response.
In individuals with these conditions, the immune system overreacts when exposed to certain substances, such as specific foods or environmental triggers.
This exaggerated immune response leads to inflammation, which can manifest as skin rashes (eczema) or systemic allergic symptoms (food allergies).
The causes of this irregular immune response, possibly involving genetic, environmental, and gut microbiota factors, are not fully understood.
In people with eczema, their skin’s outermost layer becomes compromised due to genetic factors or external irritants such as harsh soaps or allergens.
The weakened barrier lets allergens penetrate deeper skin layers, triggering inflammation and itchy eczema rashes.
It is important to note that while these factors are known to contribute to food allergies and eczema, each individual’s experience may vary, and additional research is still needed to fully understand all the underlying causes.
Risk in Children
One crucial aspect of risk in children is their immature immune system.
The immune system of infants and young children is still developing, making it more prone to hypersensitivity reactions.
This heightened susceptibility can manifest as both food allergies and eczema.
Genetics plays a significant role in determining the risk of food allergies and eczema in children.
Studies have revealed that if one or both parents have a history of allergic conditions like asthma, hay fever, or eczema, their child is also more likely to develop these conditions.
This genetic predisposition underscores the importance of understanding and addressing the familial component when assessing the risk in children.
Research suggests that certain environmental factors during pregnancy can impact a child’s susceptibility to these conditions later on.
Maternal smoking, for instance, has been linked to an increased likelihood of both food allergies and eczema in offspring.
Exposure to allergenic foods during infancy – especially when complementary feeding begins – may influence allergic outcomes.

Common Food Triggers
1. Dairy Products
- Specific Triggers: Proteins like casein and whey in cow’s milk.
- Allergic Response: Trigger an immune response causing symptoms like redness, itching, and inflammation.
- Demographics Affected: More children have a casein allergy, while more adults may have lactose intolerance.
- Conditions Exacerbated: Can worsen eczema symptoms and flare-ups.
2. Eggs
- Specific Triggers: Proteins in egg whites, especially ovomucoid and albumin.
- Allergic Response: This can cause reactions ranging from hives and digestive discomfort to severe reactions like anaphylaxis.
- Conditions Exacerbated: Can worsen skin inflammation and itchiness in eczema patients allergic to eggs.
3. Peanuts
- Specific Triggers: Peanut proteins such as Ara h1 and Ara h2.
- Allergic Response: Trigger IgE-mediated allergic responses, leading to immediate hypersensitivity reactions.
- Conditions Exacerbated: Can exacerbate skin irritation and inflammation in eczema patients.
4. Tree Nuts
- Specific Triggers: Almonds, walnuts, cashews, pistachios, etc. Proteins like almond profilins or walnut vicilins.
- Allergic Response: This can cause symptoms ranging from mild oral allergy syndrome (itchy mouth) to severe systemic reactions including anaphylaxis.
- Conditions Exacerbated: Can worsen eczematous lesions.
5. Soy
- Specific Triggers: Proteins such as glycinin and beta-conglycinin.
- Allergic Response: Trigger allergic responses.
- Demographics Affected: More common in infants and children.
- Conditions Exacerbated: Can exacerbate eczema flare-ups, and aggravate itching, redness, and skin inflammation.
IgE-Mediated Food Allergies
When certain foods cause a strong sensitivity in people, their body makes these things called IgE antibodies.
These antibodies attach themselves to cells in different parts of the body. If the person eats the allergic food again, these antibodies order the cells to release a bunch of chemicals, like histamine, which brings on allergy symptoms.
Some might experience them immediately or within two hours after eating the allergic food.
Symptoms can include getting hives or itching, facing trouble breathing, feeling nauseous, or having low blood pressure.
In extreme cases, anaphylaxis can happen. This super serious condition makes breathing really hard and causes a big drop in blood pressure.
It’s crucial to pinpoint exactly which foods cause these reactions by doing things like skin tests or blood tests.
Common allergy-causing foods include peanuts, tree nuts like walnuts and almonds, shellfish, fish, eggs, milk products, soybeans, and wheat.
People with these allergies need to completely avoid these foods because even a tiny bit can set off a reaction.

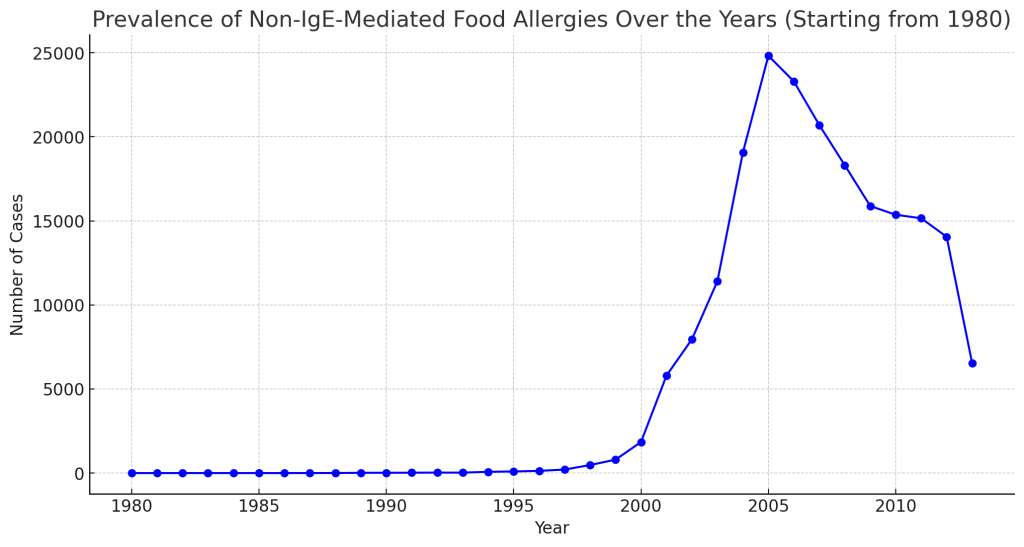
Non-IgE-Mediated Food Allergies
While most food allergies trigger a fast response and involve something called IgE antibodies, non-IgE-mediated food allergies don’t follow this path.
They use other parts of your immune system. One kind called cell-mediated or delayed hypersensitivity reaction, kicks in when certain cells in your immune system tag a part of food as an invader and go after it.
With this type, you might not see symptoms until hours or even days after you eat the food.
Common symptoms throw you into stomach troubles like vomiting, diarrhea, stomach pain, and bloody stools.
You might also notice eczema flare-ups after eating the food you’re allergic to.
Then there’s another type called mixed IgE- and cell-mediated allergy. This one hits you with both immediate and delayed reactions.
If you have this type of allergy, you might face immediate symptoms like hives or swelling, and later deal with stomach discomfort or skin rashes that look like eczema.
This complexity ramps up the difficulty in pinpointing the trigger foods, leading doctors who specialize in allergies to run numerous tests to figure it out.
Getting the lowdown on these different types of food allergies allows doctors to nail the diagnosis and find the right strategy to handle the allergy.
Treatment
While there is no cure for food allergies or eczema, various therapies can help alleviate symptoms and improve quality of life.
It typically includes a combination of medical interventions, dietary modifications, and lifestyle adjustments.
Identifying specific allergens through diagnostic testing, such as skin prick tests or blood tests, can guide dietary modifications.
Once trigger foods are identified, strict avoidance becomes key in preventing allergic reactions or exacerbation of eczema symptoms.
In cases where multiple food allergies are present, working with a registered dietitian specializing in food allergies can be tremendously helpful in crafting an appropriate meal plan that ensures adequate nutrition while avoiding allergens.

Probiotics
These live bacteria and yeasts, typically found in certain foods or supplements, are believed to promote a healthy balance of gut microbiota and modulate the immune system.
The use of probiotics as a therapeutic approach for managing food allergies and eczema has shown promise but remains an evolving field of research.
Several studies have explored the potential benefits of probiotics in preventing or reducing the occurrence of food allergies.
While these findings are encouraging, it is important to note that not all strains or combinations of probiotics may yield the same results. Different themes may have varying effects on gut microbiota composition and immune responses.
Some clinical trials have shown promising results regarding the reduction of eczema severity with certain strains of probiotics.
For instance, one study found that supplementation with Lactobacillus rhamnosus resulted in decreased eczema severity scores compared to placebo treatment.
Vitamin D
Understanding the relationship between vitamin D and eczema can help individuals with this condition better manage their symptoms.
One potential mechanism by which vitamin D affects eczema is through its immunomodulatory properties.
Eczema is characterized by chronic inflammation of the skin, so it stands to reason that adequate levels of vitamin D may help modulate immune responses and mitigate inflammation in individuals with this condition.
Studies have found that people with eczema often have lower levels of vitamin D compared to those without eczema, suggesting a possible correlation between low vitamin D levels and the development or severity of this skin condition.
Vitamin D also plays a role in maintaining skin integrity and barrier function.
The skin acts as a protective barrier against external factors such as allergens and irritants, preventing them from penetrating into deeper layers.
Consultation with a healthcare professional is advised before starting any supplementation regimen since individual needs vary based on factors such as age, overall health status, geographical location, and sun exposure.

Anti-Inflammatory Diet
An effective approach to managing both food allergies and eczema is through adopting an anti-inflammatory diet.
This dietary strategy involves consuming foods that can help reduce inflammation in the body, which may contribute to alleviating symptoms of both conditions.
The core principle of an anti-inflammatory diet is to limit or avoid foods that are known to trigger inflammation while focusing on consuming those that have anti-inflammatory properties.
It is recommended to incorporate a variety of fruits and vegetables into the diet.
These plant-based foods are rich in antioxidants, vitamins, minerals, and fiber, which can help boost the immune system and reduce inflammation.
Colorful fruits and vegetables such as berries, leafy greens, cruciferous vegetables (broccoli, cauliflower), citrus fruits (oranges, lemons), and tomatoes are particularly beneficial due to their high content of phytochemicals with anti-inflammatory effects.
Including omega-3 fatty acids in the diet is crucial for their potent anti-inflammatory properties.
Foods rich in omega-3s include fatty fish like salmon, sardines, and mackerel, as well as flaxseeds, chia seeds, and walnuts.
Incorporating sources of monounsaturated fats into the diet such as avocados and olive oil can also aid in reducing inflammation.
An anti-inflammatory diet for individuals dealing with food allergies and eczema involves prioritizing nutrient-dense fruits and vegetables, incorporating omega-3 fatty acids, choosing whole grains over refined grains, and minimizing processed sugars.

Coping
Food allergies and eczema can be challenging, but with the right strategies and support, individuals can effectively manage their condition and improve their quality of life.
Here are some key coping mechanisms to consider:
- Educate and Stay Aware:
- Educate yourself about food allergies and eczema, understanding their triggers, symptoms, and treatments.
- Actively research using reliable sources like medical websites, and books from experts, and consult with healthcare professionals.
- Keep up-to-date with current research and developments to advocate effectively for yourself and your loved ones.
- Build a Support Network:
- Surround yourself with supportive family, friends, and healthcare professionals, and join relevant support groups or online communities.
- Share experiences, exchange tips, offer emotional support, and connect with others facing similar challenges to combat feelings of isolation.
- Manage Itchiness:
- Moisturize regularly using emollients designed for sensitive skin to alleviate dryness and control itchiness.
- Skip long, hot showers or baths to prevent skin from drying out further.
- Prioritize Emotional Well-being:
- Engage in activities like meditation, yoga, journaling, or therapy to reduce stress.
- Talk about your concerns with healthcare professionals or join support groups that focus on the psychological impacts of food allergies and eczema.
- Seek professional assistance when challenges arise to enhance your quality of life.
Prevention
By taking proactive measures, individuals can reduce the risk of further complications and improve their overall quality of life.
Here are some effective strategies that can be implemented:
- Introduce Allergenic Foods Early:
- Start around 4-6 months of age, while continuing to breastfeed or use hypoallergenic formulas. This approach shows promise in lowering allergy onset in kids.
- Focus on common allergens like peanuts, tree nuts, eggs, milk, wheat, soy, fish, and shellfish. Kids tend to react more to these foods.
- Always consult a pediatrician or allergist before introducing these foods. They can guide the safe and timely introduction.
- Breastfeed Your Child:
- Breastfeeding offers numerous health and bonding benefits.
- By breastfeeding, you can lower your child’s risk of developing food allergies and eczema. Breast milk naturally protects against some allergies.
- Breast milk carries protective antibodies. These help guard against potential allergens.
- Aim to breastfeed exclusively for the first six months. This builds a strong immune foundation for your infant.
- Adopt Avoidance Strategies:
- If diagnosed with specific allergies, identify and avoid those triggers immediately.
- Always check ingredient labels when shopping. Hidden allergens often lurk in unexpected products.
- Exercise caution when eating out or consuming meals others prepare. Cross-contamination remains a risk, even with the best efforts.
- Implement Environmental Control Measures:
- Dust and vacuum regularly to minimize dust mite exposure, a common allergy trigger.
- Choose hypoallergenic bedding to reduce nightly exposure to allergens.
- Control room humidity to optimal levels. This helps prevent certain allergic reactions.
- Skip strong perfumes or heavily scented products. They can trigger respiratory or skin reactions.
- Restrict pets from entering bedrooms. Their dander often triggers allergic reactions.
- Undergo Allergy Testing and Formulate Action Plans:
- Seek an allergist or immunologist for a professional consultation. They excel in pinpointing and managing allergies.
- Discover your specific food and environmental triggers. This knowledge equips you to take a proactive stance.
- Develop a personalized action plan, which might include carrying EpiPens. Preparedness can save lives during severe reactions.
- Inform close contacts about your allergies and set precautions in places like schools or workplaces. A knowledgeable support system helps maintain a safer environment.
A Word from HealthyVibe
Food allergies and eczema are complex conditions that require careful management and understanding.
While living with both food allergies and eczema presents its own challenges, it is crucial to remember that there are resources available for support.
By staying informed about current research and working closely with healthcare providers, individuals can navigate these conditions successfully.
With proper management strategies in place – including avoiding known allergens or triggers – many people living with these conditions experience significant improvements in their overall well-being.













