Table of Contents
ToggleWhat are IgE-mediated food allergies?
IgE-mediated food allergies are a specific type of allergic reaction triggered by the immune system’s response to specific proteins found in food.
These food allergies arise when the immune system mistakenly identifies harmless food proteins as threats.
This misidentification goes against the immune system’s usual role of defending against actual harmful elements like bacteria and viruses.
When your body thinks a food protein is harmful, it produces something called immunoglobulin E (IgE) antibodies.
These antibodies bind to specific cells, prompting them to release chemicals that trigger allergic symptoms. Symptoms can range from mild issues like itching and hives to severe, potentially life-threatening anaphylaxis.
Now, why does this happen? It seems like a mix of your genes (your family’s health history) and your environment (like early exposure to certain foods) play a role. If your family has a history of allergies or asthma, you might be more likely to develop food allergies.
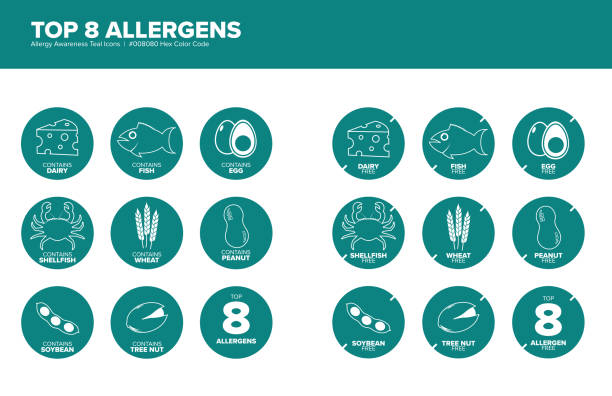
What’s more, contact with even a tiny bit of the food you’re allergic to can cause a reaction. Some common foods that people are allergic to include peanuts, tree nuts, milk, eggs, soybeans, wheat, fish, and shellfish.
Causes of IgE-mediated food allergies
Imagine your immune system is like a security system of a building. It is always on the lookout for harmful things like bacteria and viruses, to protect your body.
In some people, this security system mistakenly thinks harmless things, like certain foods, are dangerous and tries to fight them off. This is known as a food allergy.
In a type of food allergy called IgE-mediated food allergy, a part of the immune system called Immunoglobulin E (IgE) is involved.
Think of IgE as the security guards. In some people, their security guards overreact to harmless foods by releasing chemicals that cause allergy symptoms.
There are many reasons why some people have this type of allergy:
Genetics (Born with It):
Just like you inherit the color of your eyes or hair from your parents, some people inherit a higher chance of getting food allergies.
Certain genes, which are like instructions in your cells, can make you more likely to have allergies.
If these genes have errors or mutations, it can make your immune system more sensitive.
Early Exposure to Foods:
Imagine if the first time a security guard saw something, they were told it was dangerous.
They might always believe it’s dangerous from then on. Similarly, when babies are first introduced to foods, how and when they are introduced can influence whether their immune system sees the food as a friend or foe.
Environmental Factors:
Things in your environment, like air pollution or cigarette smoke, can also affect your immune system.
For example, breathing in a lot of pollution might make your immune system more sensitive and more likely to overreact to foods.

Pre-existing Conditions:
People with other allergies or conditions like asthma (a lung condition) or eczema (a skin condition) might be more likely to develop food allergies.
This is because their immune system is already sensitive.
Understanding IgE-Mediated Food Allergy Signs and Symptoms
SIgE-mediated food allergies are a type of food allergy that can cause different signs and symptoms for different people.
They’re kind of unpredictable. Some people might have a mild reaction, while others might end up in a really serious, life-threatening situation.
One of the main signs that you’re dealing with an IgE-mediated food allergy is if you suddenly start itching and break out in hives shortly after eating a certain food.
Hives look like raised, red bumps on your skin that can be super itchy and uncomfortable. Sometimes they even burn. They can show up anywhere on your body – your face, neck, torso, arms, and legs.
Another symptom you might get is angioedema, which is a fancy term for when the deeper layers of your skin start to swell.
Unlike hives, which are on the surface, angioedema can cause swelling under your eyes, or on your lips and tongue. It’s usually not painful, but it can make you really uncomfortable, especially if it affects your face or makes it hard for you to talk or swallow.
Some people with these food allergies might have trouble breathing because their airways get inflamed when they eat foods they’re allergic to.
This is really serious and a big deal because it involves important breathing organs. Some people might also get stomach issues like abdominal pain, nausea, vomiting, or diarrhea.
You definitely shouldn’t ignore these symptoms. They can get worse fast and lead to anaphylaxis, which is a severe allergic reaction that needs immediate medical attention.

Testing & Diagnosing IgE-Mediated Food Allergies
A thorough evaluation typically involves a combination of medical history, physical examination, and specialized tests.
Two commonly used tests for the diagnosis of these allergies are the skin test and the blood test.
The skin test is a reliable method to identify specific allergens that trigger an allergic reaction. During this procedure, small amounts of allergenic extracts are applied to the skin’s surface through tiny pricks or scratches.
Commonly tested allergens include peanuts, tree nuts, eggs, milk, soy, wheat, fish, and shellfish.
If an individual has sensitization to any of these substances, they may exhibit localized reactions such as redness or swelling at the site of application.
Blood tests measure the level of specific IgE antibodies circulating in the bloodstream in response to particular food allergens.
The most frequent type of blood test used is called a radioallergosorbent test (RAST) or enzyme-linked immunosorbent assay (ELISA).
These tests detect IgE antibodies produced by immune cells that recognize specific food proteins.
The results are reported as numerical values indicating levels of sensitivity or classifying them into categories like low (class I), moderate (class II), high (class III), very high (class IV), or extremely high (class V).
These categorizations help healthcare professionals determine if a person has sensitization to certain foods and guide them in developing appropriate dietary restrictions.

Skin Test for IgE-Mediated Food Allergies
A skin test is a common diagnostic tool used by allergists to determine if an individual has IgE-mediated food allergies.
This simple and non-invasive procedure involves applying small amounts of allergen extracts onto the surface of the skin and observing any allergic reactions that may occur.
The test is typically performed on the forearm or back, as these areas provide enough space to test multiple allergens simultaneously.
To conduct a skin test, the allergist first cleans the area with alcohol to ensure no contaminants interfere with the results. They then gently scratch the skin with a sterile lancet or tiny needle, applying specific food allergens onto each mark.
Common food allergens tested include peanuts, tree nuts, milk, eggs, wheat, soy, fish, and shellfish.
Following the application of the allergens, patients are closely monitored for about 15-20 minutes for any signs of an allergic reaction.
The presence of characteristic symptoms like redness (erythema), swelling (wheal), itchiness (pruritus), or raised bumps (hives) indicates a positive reaction to that particular allergen.
The size and severity of these reactions are measured and recorded by medical professionals to assess their significance.
It is important to note that although skin tests are highly accurate in identifying IgE-mediated allergies, false positives can occasionally occur due to other factors such as medications or underlying skin conditions.

Blood Test for IgE-Mediated Food Allergies
Also known as specific IgE testing or allergen-specific IgE testing, this method measures the levels of allergen-specific antibodies in the bloodstream.
The primary goal of a blood test is to identify and quantify the presence of immunoglobulin E (IgE) antibodies that are produced in response to particular food allergens.
During a blood test, a small sample of blood is drawn from the patient’s arm and sent to a laboratory for analysis.
The lab technicians will examine the blood sample for specific IgE antibodies related to commonly implicated food allergens such as peanuts, tree nuts, eggs, milk, shellfish, wheat, and soy.
The levels of specific IgE antibodies detected in the blood can help determine if an allergy is present and how severe it may be. Generally, higher levels indicate a higher likelihood of experiencing symptoms upon exposure to that particular food allergen.
In addition to providing insight into sensitivity levels towards various food allergens, blood tests also serve other crucial purposes within allergy diagnosis.
These tests can help differentiate between genuine allergies and other conditions with similar symptoms such as intolerance or non-IgE-mediated reactions.

Treatments for IgE-Mediated Food Allergies
The primary goal of treatment is to prevent and manage allergic reactions, ensuring the safety and well-being of individuals with these allergies.
- Practice Avoidance and Make Dietary Modifications:
- Actively avoid all allergenic food(s) to manage IgE-mediated food allergies effectively.
- Educate yourself thoroughly about reading food labels and identifying hidden sources of allergens.
- Understand cross-contamination risks during food preparation and make necessary dietary modifications, such as finding alternative foods, to ensure a balanced and safe diet.
- Use Epinephrine Auto-Injectors:
- Use epinephrine to counteract severe allergic reactions by constricting blood vessels and relaxing airway muscles.
- Train yourself on the correct usage of epinephrine auto-injectors like the EpiPen and carry one at all times.
- Administer epinephrine promptly during an allergic emergency to reduce the risks associated with anaphylaxis significantly.
- Take Prescribed Medications:
- Take other prescribed medications, such as antihistamines (e.g., diphenhydramine or loratadine), to alleviate mild symptoms like itching or hives.
- Use corticosteroids in more severe cases to manage prolonged symptoms effectively when other treatments do not suffice.
- Coordinate with healthcare providers to ensure appropriate prescription and usage.
- Undergo Allergen Immunotherapy:
- Undergo gradual exposure to small amounts of the allergenic food under strict medical supervision.
- Aim to desensitize your immune system, reducing the severity and frequency of allergic reactions over time.
- Ensure trained healthcare professionals in specialized settings conduct this treatment due to potential risks.
- Work closely with Healthcare Providers:
- Collaborate closely with healthcare providers, including allergists or immunologists, for personalized and effective treatment plans.
- Schedule regular follow-up visits and ensure ongoing monitoring for assessing treatment efficacy and making necessary adjustments.
- Prioritize this ongoing partnership to ensure an optimal quality of life and enhanced safety while managing these allergies.
When to Call 911 if You Have Food Allergies
These types of allergies can lead to anaphylaxis, a severe and potentially life-threatening allergic reaction that requires immediate medical attention.
Anaphylaxis occurs rapidly and can affect various systems in the body, including the respiratory, cardiovascular, gastrointestinal, and cutaneous systems.
One of the key indicators of anaphylaxis is difficulty breathing or wheezing. This may manifest as shortness of breath, chest tightness, or a persistent cough.
Swelling in the throat or tongue can occur rapidly and cause a feeling of suffocation. If you notice any signs of respiratory distress during or after consuming a known allergen or suspect exposure to one, it is essential to call 911 immediately.
Anaphylaxis can result in a sudden drop in blood pressure (known as hypotension), leading to dizziness, lightheadedness, or even loss of consciousness.
If you observe these symptoms alongside other signs of an allergic reaction like hives or swelling on the skin following consumption of a known allergen, it is vital not to delay in seeking emergency medical assistance.
Symptoms such as difficulty breathing/wheezing and a drop in blood pressure are clear indications that immediate medical intervention is necessary.
It’s crucial for individuals with these allergies and their caregivers to be well-informed about these signs so they can respond swiftly by contacting emergency services without hesitation.
Outlook for IgE-Mediated Food Allergies
While it can be challenging to predict the exact course of these allergies, there are several factors that can provide insight into the overall outlook.
Firstly, it is important to note that many children with IgE-mediated food allergies are likely to outgrow them over time.
Studies have indicated that up to 70-80% of children with milk, egg, soy, and wheat allergies will eventually develop tolerance to these allergens by school age.
This is particularly encouraging news for young children who often experience significant restrictions in their diet and daily life due to these allergies.
When it comes to certain allergens such as peanuts, tree nuts, fish, and shellfish, the likelihood of outgrowing the allergy decreases significantly.
Research suggests that only around 20% of children affected by peanut allergy will eventually become tolerant to this allergen.
Similarly, the rates for outgrowing tree nut allergies range between 10-14%, while only about 4-5% of individuals allergic to fish or shellfish acquire tolerance over time.
Having multiple food allergies or co-existing atopic conditions like asthma or allergic rhinitis may also influence prognosis and require more comprehensive management strategies.

Current Research for IgE-Mediated Food Allergies
Advancements in medical research have shed light on various aspects of IgE-mediated life-threatening food allergies.
Researchers are now working to understand the fundamental mechanisms behind allergies. This knowledge is used to develop new treatments, enhancing the lives of those affected.
Scientists have identified several genetic factors that may contribute to an individual’s susceptibility to these allergies.
Recent studies have found that variations in certain genes involved in immune regulation and allergic responses can increase the risk of developing IgE-mediated food allergies.
By unraveling the genetic basis of these allergies, researchers hope to develop personalized treatments that target specific genes or pathways implicated in allergic reactions.
Immunotherapy, which aims to desensitize individuals by gradually exposing them to small amounts of allergenic proteins, is one area garnering considerable attention.
Ongoing clinical trials are assessing different immunotherapeutic strategies, such as oral immunotherapy and sublingual immunotherapy, with promising results so far.
These approaches aim to modify the immune system’s response to allergens and potentially provide long-lasting protection against severe allergic reactions.
There is increasing interest in exploring alternative treatments for IgE-mediated food allergies beyond traditional medications like antihistamines and epinephrine auto-injectors.
Natural remedies and complementary therapies are being investigated for their potential benefits in reducing symptoms or preventing severe reactions.
Through these endeavors, scientists aim to enhance our understanding of these allergies and improve the quality of life for individuals affected by them.

A Word From HealthyVibe
Everyone needs to understand and manage severe food allergies. Know the signs, get the right tests and diagnosis, and find the best ways to treat the allergies.
Don’t forget, preventing allergies is key.
Learn how to avoid allergens, read labels, and stop cross-contamination to lower the chances of accidentally coming into contact with allergens.
Also, make sure to have an emergency plan. Always carry an epinephrine auto-injector, know how to use it, and inform close friends and family about the allergy.
Even though it’s tough living with severe food allergies, don’t lose hope. Use the right strategies and get support from healthcare pros to live a happy, full life.









